Alzheimer’s disease is a progressive neurological disorder that primarily affects older adults, leading to memory loss, impaired judgment, and eventually a decline in the ability to carry out everyday tasks. Early diagnosis is crucial for managing symptoms effectively and improving quality of life. Understanding the 7-stage model of Alzheimer’s progression can help in recognizing early symptoms and seeking timely intervention. Advances in diagnostic tools have improved our ability to detect Alzheimer’s at earlier stages, offering new hope for patients and families. This article explores the 7-stage model and how new diagnostic methods can identify symptoms early on.
The 7-Stage Model of Alzheimer’s Disease
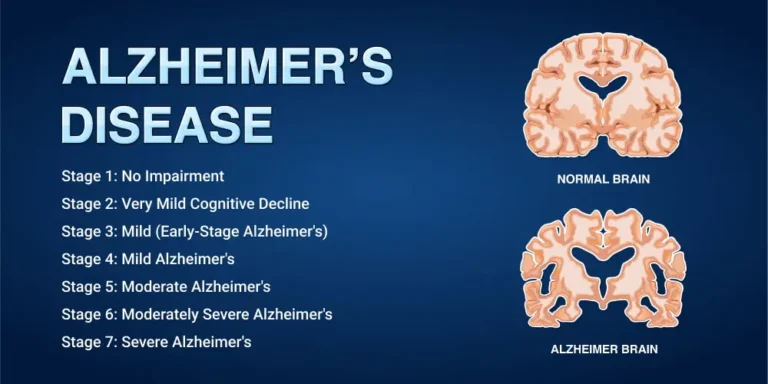
Alzheimer’s disease progresses gradually, with symptoms worsening over time. The 7-stage model breaks the disease into distinct stages, each characterized by specific changes in cognitive function and behavior. The stages are as follows:
- Stage 1: No Impairment
- Stage 2: Very Mild Cognitive Decline
- Stage 3: Mild Cognitive Decline
- Stage 4: Moderate Cognitive Decline (Mild Alzheimer’s Disease)
- Stage 5: Moderately Severe Cognitive Decline (Moderate Alzheimer’s Disease)
- Stage 6: Severe Cognitive Decline (Moderately Severe Alzheimer’s Disease)
- Stage 7: Very Severe Cognitive Decline (Late-Stage Alzheimer’s Disease)
Recognizing early symptoms in Stages 1-3 can make a significant difference in managing Alzheimer’s and slowing its progression.
Stage 1: No Impairment – The Silent Beginning
In Stage 1, there are no noticeable symptoms, and individuals appear completely healthy. However, changes are beginning to happen within the brain, including the accumulation of amyloid plaques and tau tangles, which are hallmarks of Alzheimer’s. These changes are not detectable through normal behavior or cognitive tests, but advanced imaging techniques and biomarkers can sometimes detect early alterations.
Recent advances in diagnostic imaging, such as positron emission tomography (PET) scans, allow doctors to observe amyloid plaques in the brain before symptoms arise. Additionally, biomarkers found in cerebrospinal fluid (CSF) can also indicate early signs of Alzheimer’s, even before any cognitive decline occurs.
Stage 2: Very Mild Cognitive Decline – Signs of Forgetfulness
Stage 2 is characterized by very mild memory lapses, such as forgetting familiar words or misplacing objects. These changes are often mistaken for normal aging, which makes it challenging to identify this stage as Alzheimer’s. Friends, family, and even the individual may dismiss these memory issues as a natural part of getting older.
Recent advances in cognitive testing can be helpful in distinguishing normal aging from early Alzheimer’s. Computer-based cognitive assessments can detect subtle changes in memory, language, and problem-solving skills, allowing for an earlier diagnosis. At this stage, individuals experiencing these symptoms should seek medical evaluation, particularly if they notice a pattern or progression of forgetfulness.
Stage 3: Mild Cognitive Decline – Detecting Patterns
Stage 3 is where the first significant warning signs of Alzheimer’s appear. Memory issues become more noticeable, and individuals may have difficulty finding the right words, remembering recent events, or organizing tasks. They may also struggle with making plans or feel overwhelmed by more complex activities.
Advanced neuropsychological tests are crucial at this stage to identify cognitive deficits beyond what is expected for age-related decline. Functional MRI (fMRI) scans can reveal changes in brain activity that correlate with early symptoms. At this stage, doctors may also utilize more sensitive biomarkers, including blood tests that can detect specific proteins linked to Alzheimer’s, to confirm an early diagnosis.
Recognizing Stage 3 is vital, as it represents a turning point between MCI (Mild Cognitive Impairment) and mild dementia. An early diagnosis allows individuals and their families to prepare for the future, initiate treatment, and take measures to manage symptoms.
Advances in Early Diagnosis
Recent developments in Alzheimer’s research have introduced new techniques that improve early detection:
Blood-Based Biomarkers: Advances in blood-based biomarker testing have significantly simplified the process of identifying Alzheimer’s risk. A blood test can now identify proteins like beta-amyloid and tau, which are strongly associated with Alzheimer’s disease. This development offers a less invasive and more accessible option for early diagnosis, especially during the earliest stages when no symptoms are apparent.
Genetic Testing: Genetic testing is also gaining traction for those at higher risk. Testing for the APOE-e4 gene, which is associated with an increased likelihood of developing Alzheimer’s, can help identify those at risk earlier. It’s important to note, however, that carrying the gene does not guarantee one will develop the disease, but it is a strong risk factor.
Digital Tools for Cognitive Testing: Digital cognitive assessment tools are also advancing. These tests can be administered online or via mobile applications and are designed to measure various aspects of cognitive function, including memory, attention, and language. Such tests provide a cost-effective way to track cognitive changes over time and can alert both patients and doctors to early warning signs of Alzheimer’s.
Moderate to Severe Stages: Managing Later Symptoms
As Alzheimer’s progresses beyond the early stages (Stage 4 to Stage 7), symptoms become more apparent and include confusion about time and place, significant memory loss, behavioral changes, and eventually the inability to care for oneself. Diagnosing Alzheimer’s in these later stages is often less challenging because the symptoms are more pronounced.
However, identifying the disease early on remains the primary goal for intervention. During moderate to severe stages, doctors focus on symptom management, safety, and ensuring a good quality of life for both the patient and the caregivers.
The Importance of Early Detection
Early detection of Alzheimer’s provides significant benefits. It allows for timely interventions, which may help slow disease progression and maintain cognitive function for longer. Early diagnosis also gives individuals and families time to plan for future care, explore clinical trials, and initiate treatment with medications designed to delay symptoms.
Moreover, lifestyle interventions—such as regular physical activity, a brain-healthy diet, social engagement, and mental stimulation—can be implemented earlier in the disease progression, potentially delaying the onset of severe symptoms.
Conclusion
Alzheimer’s disease progresses in seven stages, beginning with no outward symptoms and culminating in severe cognitive decline. Advances in diagnostic tools, from imaging technologies to blood biomarkers and digital assessments, have improved the ability to detect Alzheimer’s at its earliest stages, often before significant cognitive decline begins. Recognizing the early signs—such as subtle memory lapses or difficulty finding the right words—and seeking medical advice early can help individuals receive timely intervention, ultimately improving their quality of life and potentially delaying the progression of Alzheimer’s disease. Early diagnosis is the key to effective management, empowering those affected to face Alzheimer’s with knowledge, resources, and support.